Why someone pays $1000 for healthcare they can get for “free” elsewhere
“There is no more expensive thing than a free gift.”
-Michel de Montaigne
How do you know when you’ve made it?
Maybe after winning a trophy. Or landing a partner you’ll enjoy (or tolerate) for life. Or when there are enough commas in your bank account. Either way, you’re looking for a tangible moment or milestone.
Okay, then what’s the mark of a wonderful cash pay clinic, you ask? I can’t hand you a guaranteed-to-work prescription for that. But I can show you a moment proving that our clinic was on the right track.
Today’s TLDR: if you’re a cash pay clinic, hone the three C’s:
Competence. Have a maniacal emphasis on outcomes. Work both forwards to and backwards from the ideal end goals for patients.
Comfort. Make the full experience not just complete, but unhurried as well. Keep 100% attention on the patient at hand (sounds easy, but it’s not). Have contingencies in place.
Connection. Maintain consistent points of contact and build in leeway for adjustments if things go wrong.
Wait… you want to pay for that?
A patient visited us for a $1000 medical procedure rather than choosing one of three other practices nearby where the same process would have been almost 100% covered. No, the work was not cosmetic. This was for a skin cancer excision. Given the specific cancer and its location at the time, this wasn’t an unusual procedure no one else could do. Again, you wonder, why would anyone go for a cash pay clinic here? Just like in the realm of stocks: some investors want to get the cheapest business possible (for the sake of price alone), while others pay up for perceived high-quality (but more expensive) businesses like Apple or Microsoft.
Let’s start with the key patient decision-making factors in these kinds of scenarios:
Eligibility: the patient’s health plan was cleared at the other dermatology surgeons of our choice as well as the backup surgeons we had in mind.
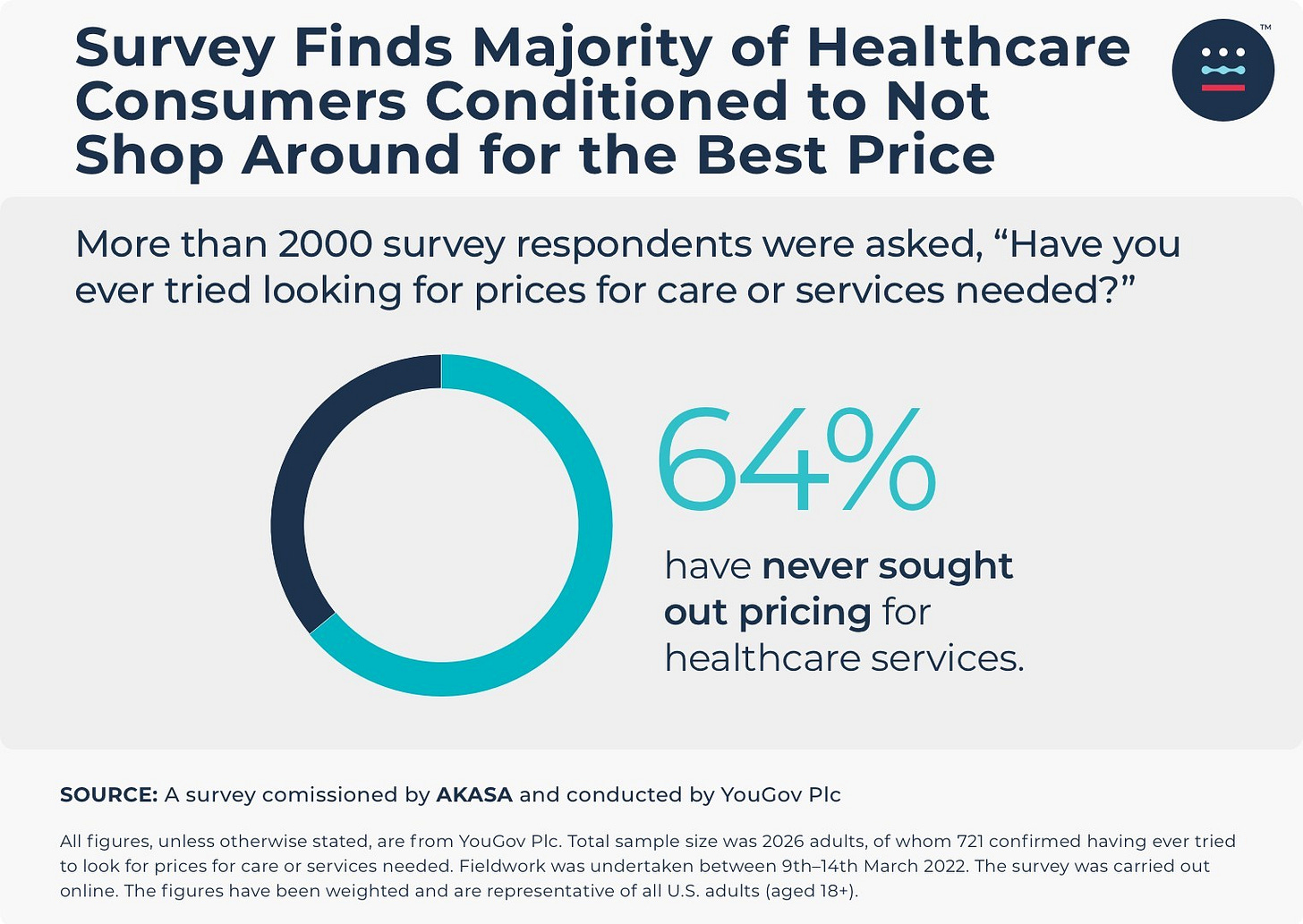
Price: this is related to insurance eligibility. Patients should know the pricing differences between options. We give quotes and estimates up front as part of our price transparency policy. Given rising deductibles among US health plans, patients may still owe thousands of dollars upfront for a procedure—regardless of the clinic. A patient should feel comfortable asking clinics what they’d bill for a routine service.
Outcomes: there’s some nuance here. The intended result (in this case the fully clear excision and skin repair) is just a baseline. But not all pre-op and post-op work is created equal. The proverbial wagon’s packed, but it still has to travel the Oregon Trail. And when it reaches the destination, there needs to be some unloading on the way to building a settlement. And so on. Hence the focus on pre-prep and long term follow-up processes. For this type of treatment, care won’t magically end after the sutures are pulled together. Skin cancer elsewhere doesn’t take a break on the account of one surgery.
Availability: sometimes it takes one to six months to visit a dermatologist in our area (I wish I was kidding). Nationally, per AMN’s most recent physician survey, wait times lean towards one month for derm. With referred skin cancer surgeries in our area, the wait can be three to nine weeks depending on the season and type of cancer. In the case of this patient, we made an opening earlier than the alternatives. But for the urgency of this procedure, that advantage was marginal.
Distance: this wasn’t a factor in this case. Each facility was almost equidistant from the patient’s home.
With that in mind, here’s why the patient chose to see us out-of-network
Our clinic’s advantages—the three C’s—for this patient were:
Competence: We have a maniacal focus on outcomes. Substance has to back up the trust we earn.
We work both forwards (starting at pre-op) and backwards (inverting from the ideal post-op healing + successful removal). Sure, anyone can remove the cancer, but we don’t want to leave behind a shoddy repair job. Not to mention that guidance shouldn’t stop after the sutures come out. There are set points of contact at day zero, seven, 14, and then adjusting from there based on healing.
We ensure that our skin cancer patients have their post-op follow ups set in advance (per medical guidelines) to catch any possible recurrences/other cancers. This all serves to maintain a rigorous pre- and post-op plan going far beyond lip service.
Comfort: We purposefully build in extra buffer time for if the procedure takes a bit longer than expected. Are we giving up time to squeeze in a brief visit with another patient? Potentially. Billing the work appropriately to account for contingencies mitigates that risk. The last persona we want to embody is the rushed surgeon watching the clock with one hand on the scalpel and another on the doorknob. But for our patients, it’s obvious that more than 100% of the doctor’s attention is on them.
Connection: Surgery is a funny thing sometimes—the best intentions can still precede terrible results. Hence why we make ourselves easy to reach after the procedure. Whoever ran the procedure (in this case our dermatologist) speaks with the patient personally for high-level decisions. This isn’t hard, but most offices (cash-based or otherwise) won’t do it. We’ve found it strange for the main care team to remove and/or treat the cancer but have the receptionist relay everything to patients. Get the easy buckets—but still delegate when necessary.
Socio-economic position alone cannot fully explain the behavior. In this case the patient did not have financial resources much beyond the national average for income and savings. Most people, even with vast resources, select the cheapest option delivering similar results. Note that similar does not equal same. Apples of two varieties differ in taste, consistency, etc. But they’re still apples. If they have a choice, patients will choose the particular apple they want. These crossroads are no different from the patient’s choice to visit us for surgery. This assumes patients know how to shop for care. In reality, not enough do.
Remember… it’s about the ideal patients
Of course, keep in mind the fact that today’s story is one of several instances at our clinic alone. We don’t pretend that all patients will pick out-of-network local surgery over something that’s covered. Not everyone has the spare funds—or considers their healthcare a top priority. Any cash pay clinic remembers that. But any elite cash pay practice serves the patients able and willing to pay for the services on offer because that clinic is a great fit.
Observe why patients choose you…
…when most would otherwise use their insurance. Note those patterns. Worrying about outcomes alone is like reading the box score without seeing the actual game. These moments you have with patients demonstrate a solid cash pay foundation. But that shouldn’t be good enough. Care to Cash guides you on how to aim ever higher, and execute on those goals, while also showing patients alternatives to insurance-based medicine. Reach us on our Substack or contact me directly @caretocash on x.com to get help finding a cash pay doctor or address questions for your practice.